Dental Insurance Claim Approvals
Why automate?
How Cflow Can Help Automate the Process:
Automated Claim Verification :
Insurers can easily set up automated verification processes for dental insurance claims as per preset business rules with Cflow. This automation reduces manual errors and speeds up the claim approval process, ensuring timely reimbursements. Cflow seamlessly integrates with dental practice management systems for automatic verification of the services rendered and cross-check them against the policyholder’s coverage.
Enhanced Compliance Checks :
Processing of dental insurance claims needs to be carried out according to regulations and policies. Cflow automates the compliance verification process so that insurers can rest easy with the assurance that each claim is in line with industry standards. The risk of non-compliance and legal issues is mitigated by automation.
Real-Time Reporting and Analytics :
Insurance personnel get real-time updates on each dental claim via the intuitive dashboard in Cflow. Cflow provides transparency and deeper visibility into the status of each claim, which helps identify potential issues and make data-driven decisions to improve efficiency. Real-time analytics also allow insurers to identify trends and optimize their processes for better performance.
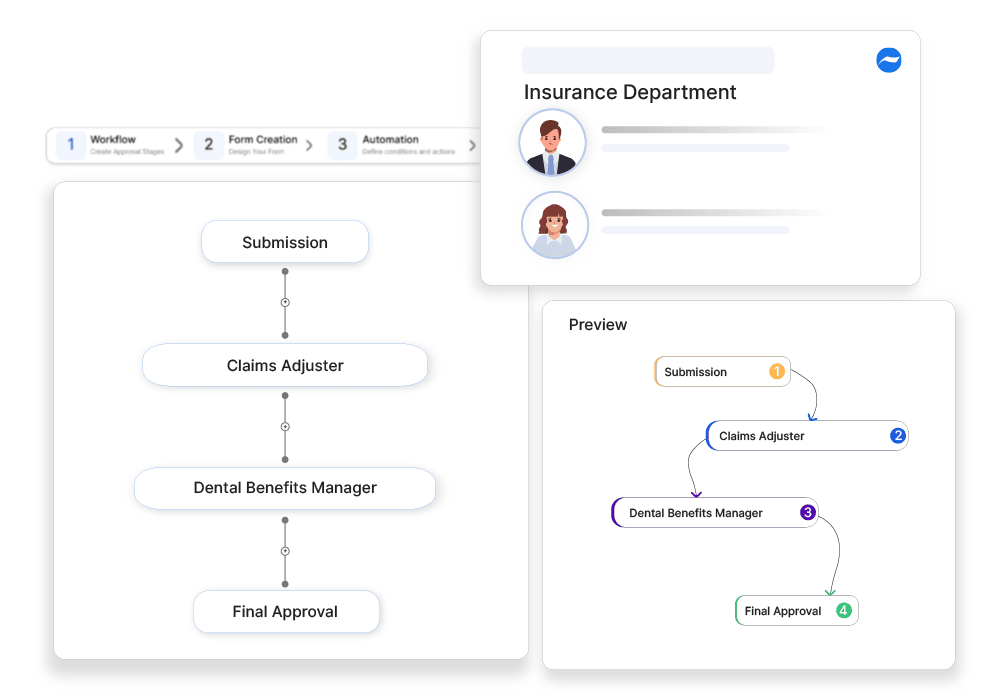
Customized Workflow Templates :
Cflow eliminates the need for coding by using visual elements to create workflows. Users can easily create approval workflows by simply moving visual elements as per preset business rules. These templates can include automated steps for document collection, eligibility checks, and final approvals, ensuring a seamless and efficient process from start to finish.
Frequently Asked Questions
What is a dental insurance claim?
A claim filed for reimbursement or direct payment for covered dental treatments.
What are the main challenges in dental insurance claims?
Pre-existing conditions, missing documentation, and provider network limitations.
How can businesses ensure smooth dental insurance claims?
By ensuring pre-authorization, maintaining dental records, and verifying insurance coverage.



