Health Insurance Pre-authorization
Why automate?
How Cflow Can Help:
Automated Treatment Verification:
Automatically verify treatment details and ensure compliance with policy terms. Reduce manual errors and streamline the process.
Enhanced Communication:
Provide timely updates and confirmations to policyholders and healthcare providers. Improve satisfaction with transparent and efficient pre-authorization processing.
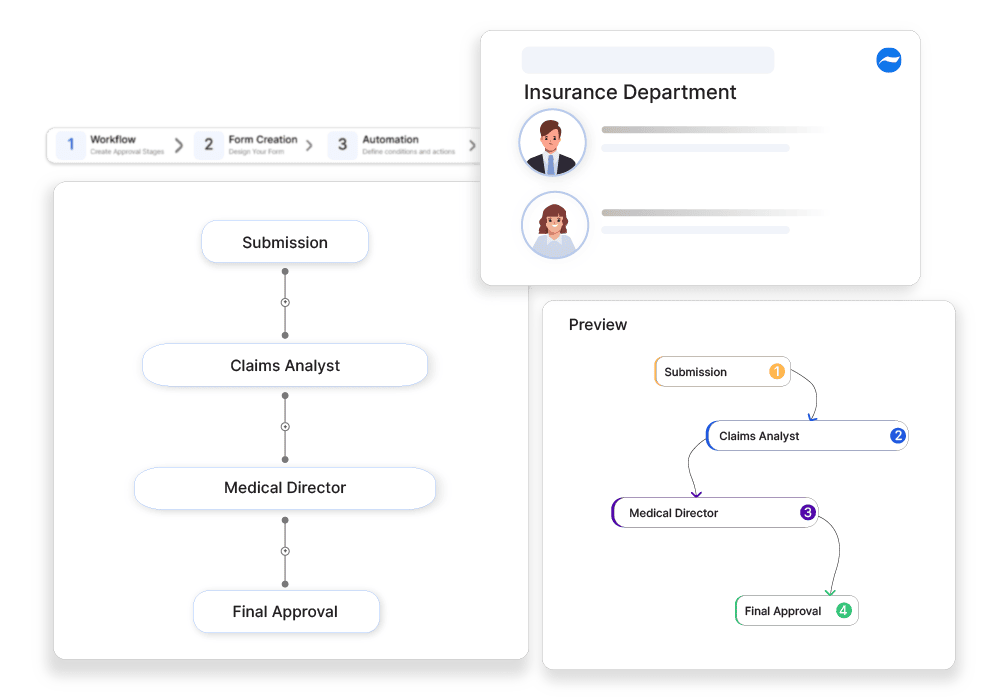
Efficient Workflow Management:
Minimize processing times and improve accuracy. Create custom workflows for managing pre-authorization approvals seamlessly.
Compliance and Record Keeping:
Maintains accurate records for audit purposes. Makes sure that all pre-authorizations comply with regulatory requirements and company policies.
Frequently Asked Questions
What is health insurance pre-authorization?
A process where insurance providers approve specific medical treatments or procedures before they are performed to confirm coverage.
What are the main challenges in health insurance pre-authorization?
Delays in approvals, strict documentation requirements, and denials due to policy exclusions.
How can businesses ensure smooth health insurance pre-authorizations?
By using electronic prior authorization systems, ensuring proper documentation, and working closely with healthcare providers.



