Pharmacy Benefit Approvals
Why automate?
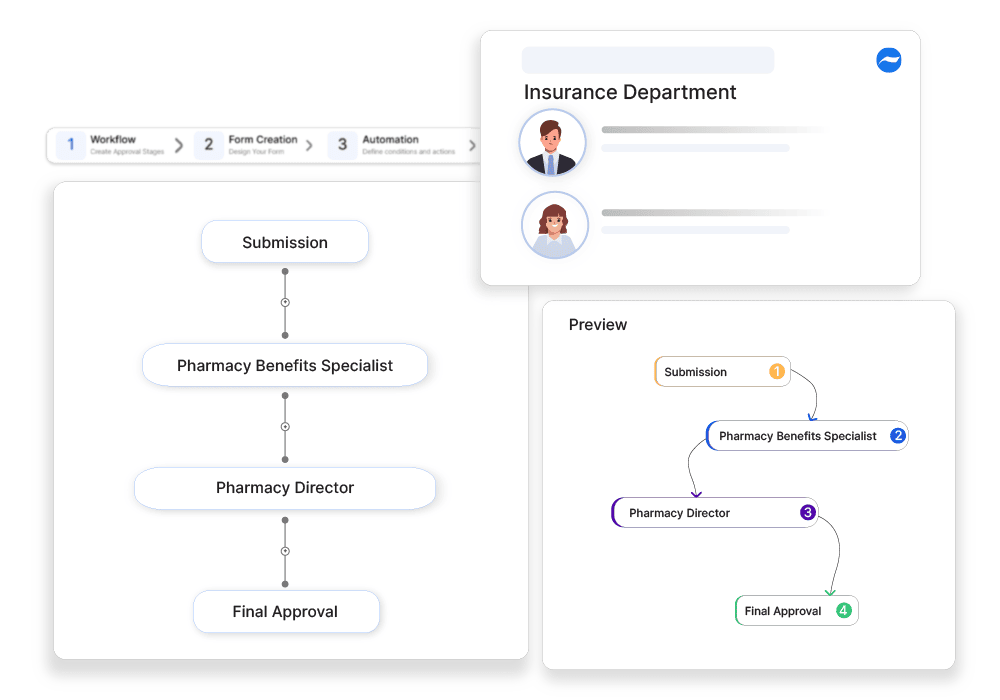
How Cflow Can Help Automate the Process:
Streamlined Formulary Checks :
Cflow can be used to automate formulary checks within the approval workflow. This ensures that only medications covered under the patient’s plan are approved.
Automated Prior Authorization :
Cflow automates the prior authorization process by integrating with pharmacy systems and the workers. This ensures that all necessary approvals are obtained.
Compliance Management :
Cflow helps with stringent regulatory requirements. This ensures that insurers stay compliant by incorporating automated compliance checks into the workflow.
Real-Time Communication :
Cflow offers a real-time communication feature where companies can facilitate collaboration and communication. This ensures that issues or questions are addressed immediately.
Frequently Asked Questions
What is a pharmacy benefit approval?
A process ensuring that prescribed medications are covered under an insurance plan.
What are the main challenges in pharmacy benefit approvals?
Prior authorization delays, formulary restrictions, and high drug costs.
How can businesses ensure smooth pharmacy benefit approvals?
By using e-prescriptions, verifying coverage before dispensing, and negotiating bulk pricing.



