Healthcare Contract Management: A Complete Guide For Providers And Administrators


Cflow Team
Share this Content
Key takeaways
- Healthcare contract management ensures that agreements between providers, payers, and vendors are efficiently created, tracked, and renewed to maintain compliance and operational efficiency.
- A contract lifecycle management system helps hospitals and healthcare organizations manage complex agreements, reducing errors and avoiding costly compliance breaches.
- Effective medical contract management streamlines negotiations, tracks performance, and enables better decision-making based on real-time contract data.
- Automated workflows in contract administration save time, reduce human error, and improve transparency throughout the contract lifecycle.
- Centralized contract repositories allow healthcare organizations to monitor key dates, renewals, and compliance obligations without missing critical deadlines.
Healthcare contract management refers to the process of creating, reviewing, executing, and tracking contracts between healthcare organizations and their stakeholders, including payers, suppliers, physicians, and service providers. In the highly regulated healthcare industry, contract management plays a crucial role in ensuring that agreements comply with legal requirements, align with organizational goals, and deliver value.
Contracts in healthcare cover a wide range of agreements, from managed care contracts with insurance companies to vendor contracts for medical equipment and service level agreements with technology providers. Managing these contracts effectively requires clear processes, strong compliance oversight, and technology that can handle the complexity of healthcare-specific terms.
This blog explores what healthcare contract management is, why it is essential, the key elements of a strong contract management process, technologies used in contract lifecycle management, challenges faced by healthcare organizations, and best practices for success.
What Is Healthcare Contract Management
Healthcare contract management is the structured process of handling contracts throughout their lifecycle, from initial drafting and negotiation to execution, monitoring, and renewal. It ensures that all contractual obligations are met, risks are minimized, and compliance requirements are adhered to.
In healthcare, these contracts often involve sensitive patient data, financial arrangements, and regulatory compliance, making the stakes higher than in many other industries. An effective contract management process not only reduces legal and operational risks but also supports better relationships between healthcare providers, payers, and vendors.
The process typically involves several stages, including drafting contract terms, internal review and approval, negotiation with external parties, execution of the agreement, monitoring of obligations and performance, and eventually, contract renewal or termination. With the right system in place, each of these stages is streamlined to avoid bottlenecks and ensure transparency.
Table of Contents
Importance Of Healthcare Contract Management
Managing contracts efficiently is essential for maintaining compliance with healthcare regulations such as HIPAA in the United States. Failure to adhere to contract terms can result in financial penalties, operational disruptions, and reputational damage.
Beyond compliance, contract management impacts revenue cycle performance. For example, inaccurate payer contracts or missed deadlines for renegotiation can lead to underpayments or claim denials. Similarly, poorly managed vendor contracts can result in higher costs or supply shortages.
An organized contract management process enables better visibility into active agreements, helping decision-makers identify cost-saving opportunities, improve negotiation outcomes, and prevent revenue leakage. It also ensures that stakeholders are aware of their responsibilities, timelines, and deliverables.
Challenges in Healthcare Contract Management
The consequences of contract management can be severe and far-reaching. Healthcare providers lose an estimated $157 billion annually due to inefficiencies in contract management. Here is a look at the main challenges faced by healthcare providers in managing contracts that obstruct strategic initiatives, missed opportunities, and disruptions in care delivery.
Challenge 1- Stemming Revenue leakage from underpayments and denials
The revenue leakage that stems from inefficient contract management is one of the most pressing issues that healthcare organizations are facing. Payment errors are one of the largest contributors to revenue leakage. According to the American Medical Association, claims processing errors by both public and private payers exceed 19%, leading to underpayments and delayed reimbursements.
Challenge 2 – Overcoming Operational Bottlenecks from Manual Processes and Lack of Standardization
Despite the high stakes associated with manual processing, several healthcare organizations still manage their complex contract portfolios using outdated manual methods. The operational bottlenecks created by manual processes result in misfiled documents, missed renewals, and unaddressed contract terms.
Challenge 3 – Ensuring Compliance with Stringent Regulatory Mandates
Healthcare contracts are governed by a web of federal and state laws designed to protect patients and ensure fairness. As per Forbes, missteps like failing to comply with Stark Laws exceptions, missing required Business Associate Agreements under HIPAA, can lead to severe legal and financial consequences.
Challenge 4 – Mastering the Value-Based Care (VBC) Contract Performance
There is an ongoing fundamental shift today in healthcare payments, leaning towards Value-Based Care (VBC) from Fee-For-Service (FSS). This allows providers to be reimbursed based on the quality of outcomes of care, rather than the volume of services delivered. Barriers to embracing VBC include infrastructure requirements for data analytics, quality metrics, financial risk, workflow and culture, and administrative complexity.
Key Elements Of Effective Healthcare Contract Management
An effective healthcare contract management system combines clear processes, secure storage, and automated oversight to ensure that agreements are executed, monitored, and renewed without disruption. Each element works together to provide full visibility over contractual obligations and to minimize legal, financial, and operational risks.
1. Centralized contract repository
A centralized repository is the foundation of efficient contract management. By storing all agreements in one secure, searchable location, healthcare organizations eliminate the risk of misplaced or duplicate documents. A single source of truth also allows authorized users across departments, such as legal, finance, procurement, and clinical operations, to access the most up-to-date contract versions. In a hospital setting, this ensures that payer contracts, physician agreements, and vendor contracts are easily retrievable when needed for audits, renewals, or dispute resolution.
2. Clear approval workflows
Well-defined approval workflows ensure that every contract is reviewed and signed off by the right stakeholders before execution. In healthcare, this may involve multiple layers of review, including legal teams for compliance, finance teams for budget approval, and department heads for operational alignment. Automated workflows can route contracts to the appropriate parties in sequence, track progress in real time, and reduce bottlenecks caused by manual handoffs.
3. Compliance tracking
Healthcare contracts often involve strict regulatory requirements, such as HIPAA for patient privacy, Stark Law for physician arrangements, or state-specific licensing obligations. Compliance tracking ensures that every clause, term, and deliverable meets legal and industry standards. Automated systems can flag potential non-compliance issues early, monitor key performance metrics, and maintain a full audit trail, making regulatory audits smoother and less time-consuming.
4. Performance monitoring
A contract is only as valuable as its execution. Performance monitoring involves regularly assessing whether vendors, payers, or service providers are meeting their contractual obligations. For example, a managed care agreement might require specific claims turnaround times, while a medical equipment vendor may have uptime guarantees for leased devices. Tracking these commitments helps identify underperformance early and gives organizations the opportunity to renegotiate or enforce penalties.
5. Automated alerts and notifications
One of the most common causes of missed opportunities or penalties in healthcare contract management is failing to act on key dates. Automated alerts can notify relevant teams when contracts are approaching expiration, when renewal deadlines are near, or when performance review milestones are due. These reminders help avoid lapses in service, last-minute renegotiations, and missed compliance deadlines that could impact operations or reimbursement.
6. Data-driven reporting and analytics
Advanced contract management systems provide reporting tools that deliver insights into contract volumes, performance metrics, compliance rates, and financial impacts. For healthcare executives, having access to these analytics supports more informed decision-making—such as identifying cost-saving opportunities, optimizing vendor relationships, and negotiating better contract terms in the future.
7. Integration with other systems
Contracts do not exist in isolation. Integrating contract management software with other healthcare systems, such as electronic health records, procurement platforms, and financial management systems, ensures that data flows seamlessly between departments. This reduces the need for duplicate data entry, improves accuracy, and provides a more complete view of how contractual obligations align with patient care and operational goals.
Types Of Contracts In Healthcare
Healthcare organizations manage a wide range of contracts that cover relationships with payers, providers, suppliers, and other stakeholders. Each contract type serves a specific purpose and requires careful oversight to ensure compliance, financial accuracy, and operational efficiency.
Payer-provider agreements
These contracts define the terms under which healthcare providers deliver services to patients covered by an insurance plan. They specify reimbursement rates, billing procedures, covered services, and prior authorization requirements. Effective management of these agreements is critical to ensure timely payments and avoid revenue loss from underpayment or claim denials.
Physician employment contracts
Hospitals and clinics use these contracts to formalize relationships with employed or affiliated physicians. They typically cover job responsibilities, compensation models, benefits, schedules, non-compete clauses, and compliance obligations. Well-drafted physician contracts help attract talent while ensuring legal compliance with regulations such as the Stark Law and the Anti-Kickback Statute.
Vendor and supplier contracts
These agreements govern the procurement of medical equipment, pharmaceuticals, IT systems, and other goods and services needed to operate healthcare facilities. They outline pricing, delivery schedules, warranties, service levels, and penalties for non-performance. Managing these contracts effectively ensures supply chain reliability and cost control.
Managed care contracts
Managed care organizations, such as HMOs and PPOs, negotiate contracts with healthcare providers to control costs and improve care coordination. These contracts often involve risk-sharing arrangements, performance-based incentives, and strict reporting requirements. Managed care contracts that are poorly managed can impact both patient access and financial stability.
Service level agreements (SLAs)
SLAs define the expected performance standards between a healthcare organization and a service provider, such as IT support, cleaning services, or outsourced clinical services. They include measurable metrics like response times, uptime guarantees, and quality benchmarks. Monitoring SLAs helps ensure service providers deliver consistently and meet operational needs.
Research and clinical trial agreements
These contracts are used when healthcare organizations collaborate with research institutions or pharmaceutical companies on clinical trials. They address funding, data ownership, intellectual property rights, patient consent, and compliance with ethical and regulatory standards. Proper management ensures research integrity and legal protection for all parties.
Medical equipment lease agreements
Instead of purchasing equipment outright, some healthcare organizations lease devices like imaging machines or surgical tools. Lease agreements detail rental terms, maintenance responsibilities, usage limits, and end-of-lease conditions. Managing these agreements prevents unexpected costs and ensures continuous access to essential equipment.
Consulting and professional services contracts
These agreements outline the scope, deliverables, fees, and confidentiality obligations when engaging consultants, trainers, or other professionals. They help ensure that external expertise is aligned with the organization’s goals and regulatory requirements.
Technologies In Healthcare Contract Lifecycle Management
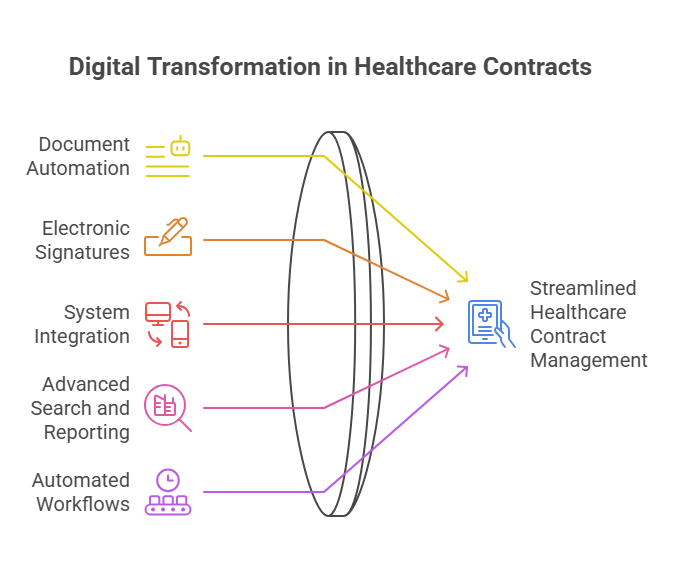
Modern healthcare contract management often relies on specialized contract lifecycle management (CLM) software. These platforms support the entire process from drafting to renewal and include features such as:
Document automation: Templates and clause libraries enable faster and more consistent contract drafting.
Electronic signatures: Digital signing capabilities allow for quick, secure execution of agreements without delays.
Integration with other systems: Linking CLM software with electronic health records, financial systems, and procurement platforms ensures data consistency and reduces duplicate work.
Advanced search and reporting: Powerful search tools and customizable reports give decision-makers quick insights into contract obligations, risks, and performance.
Automated workflows: Task assignments, notifications, and approval routing reduce manual intervention and speed up contract cycles.
End-to-end workflow automation
Build fully-customizable, no code process workflows in a jiffy.
How Cflow Automates Contract Approval
Cflow streamlines the contract approval process for healthcare organizations by replacing manual, paper-based workflows with a fully digital and automated system. This reduces delays, minimizes errors, and ensures that every agreement passes through the right review channels before execution.
The process begins with contract initiation, where a user uploads or creates a draft contract directly in Cflow’s secure environment. The platform routes the contract automatically to the relevant stakeholders, such as legal, finance, compliance, and department heads, based on predefined rules. This eliminates the need for constant follow-up emails or physical document transfers.
Cflow’s visual workflow builder allows organizations to customize the approval sequence to match internal policies. Parallel or sequential approvals can be configured, ensuring that contracts move efficiently through multiple reviewers without unnecessary bottlenecks. Each step in the workflow is time-stamped, providing a clear audit trail for compliance purposes.
Automated notifications and reminders keep all stakeholders informed of pending tasks, reducing the risk of missed deadlines. If a reviewer takes no action within the allotted time, the system can escalate the approval request to the next level, ensuring that critical agreements are not stalled.
In addition to speeding up approvals, Cflow integrates compliance checks into the process. The system can verify that required clauses, such as HIPAA compliance statements, payment terms, and service level expectations, are included before a contract moves to the signing stage. This prevents costly legal revisions and ensures that all agreements meet organizational and regulatory requirements.
Once approvals are complete, Cflow can integrate with e-signature platforms to finalize the contract digitally, enabling same-day execution. The approved document is then stored in a centralized repository within Cflow, making it easy to retrieve for audits, renewals, or performance monitoring.
By automating contract approval, Cflow enables healthcare organizations to reduce administrative overhead, improve compliance, and accelerate time-to-signature, which allows them to focus more on delivering quality patient care and less on paperwork.
Best Practices For Healthcare Contract Management
Successful healthcare contract management is built on a foundation of structured processes, transparency, and proactive oversight. Implementing best practices not only improves compliance and operational efficiency but also helps healthcare organizations maximize the value of every agreement.
1. Implement a centralized contract management system
A centralized system consolidates all contracts into a single secure repository, eliminating the risks of lost documents or outdated versions circulating among teams. In healthcare, where contracts range from physician employment agreements to vendor service contracts and payer-provider agreements, a centralized system ensures that authorized staff can quickly locate the correct version when needed. This approach reduces administrative overhead and improves collaboration across legal, procurement, finance, and operational teams.
2. Standardize contract templates and clauses
Consistency in language, structure, and legal terms reduces the time spent drafting and reviewing contracts. Standardized templates and pre-approved clauses also minimize legal risks by ensuring that all agreements meet the organization’s compliance requirements. For example, standardized clauses can address HIPAA compliance, service level expectations, or dispute resolution processes in a uniform way across all vendor contracts. This speeds up negotiations and lowers the likelihood of introducing non-compliant language.
3. Train staff on contract management procedures
Even the most advanced contract management system is ineffective if the people using it are not well-trained. Regular training sessions ensure that staff understand the correct procedures for drafting, reviewing, approving, and storing contracts. Training should also cover compliance requirements and data security protocols, especially when handling contracts that include sensitive patient or financial information.
4. Automate key processes
Automation reduces the risk of human error and ensures that critical tasks, such as sending renewal reminders or flagging compliance issues, happen on time. Automated workflows can route contracts for approval, generate alerts for approaching deadlines, and trigger compliance checks before execution. For instance, if a contract is set to expire in 60 days, the system can automatically notify the relevant department to initiate renewal negotiations.
5. Conduct regular audits
Periodic contract audits allow organizations to assess performance, compliance, and financial outcomes. Audits can uncover issues such as missed deadlines, underperforming vendors, or unclaimed rebates, giving organizations the opportunity to address problems early. In healthcare, audits can also verify that payer contracts align with billing practices and that service providers meet agreed-upon quality metrics.
6. Monitor vendor and partner performance
Contracts are living documents, and ongoing performance monitoring ensures that partners deliver on their commitments. Setting measurable performance indicators, such as claims processing times, equipment uptime, or supply delivery schedules, provides a benchmark for evaluating vendor reliability. This data can guide renegotiations, renewals, or even vendor replacement decisions.
7. Maintain robust compliance oversight
Compliance is critical in healthcare contract management, given the industry’s complex legal environment. Implement processes that monitor compliance with federal, state, and local regulations, as well as industry standards. For example, ensure that physician contracts comply with Stark Law and Anti-Kickback Statute provisions. A strong compliance program reduces the risk of costly legal disputes and reputational damage.
8. Foster cross-department collaboration
Contract management touches multiple departments, including legal, finance, procurement, clinical operations, and IT. Encouraging collaboration ensures that all perspectives are considered during drafting, negotiation, and execution. Involving key stakeholders early also reduces delays and improves the quality of the final agreement.
9. Leverage analytics for continuous improvement
Advanced reporting tools can track contract lifecycle times, renewal success rates, and compliance performance. Analyzing this data helps identify bottlenecks, optimize workflows, and improve negotiation strategies. Over time, data-driven insights lead to stronger contracts and more efficient processes.
Final Thoughts
Healthcare contract management is a vital function for ensuring compliance, improving financial performance, and building strong partnerships with payers, vendors, and service providers. A well-structured contract lifecycle management process helps healthcare organizations avoid costly errors, streamline negotiations, and maintain transparency throughout the contract’s duration.
Cflow offers a no-code, AI-powered workflow automation platform that can simplify healthcare contract management from start to finish. With features like visual workflow builders, automated alerts, integration capabilities, and secure document handling, Cflow enables organizations to manage contracts more efficiently and with greater accuracy. Start your free trial with Cflow today to experience a smarter way to handle healthcare contracts.
FAQs
What types of contracts are common in healthcare?
Common contracts in healthcare include payer-provider agreements, vendor contracts for medical equipment and supplies, physician employment contracts, managed care agreements, and service level agreements with third-party providers.
How does contract management impact revenue in healthcare?
Efficient contract management ensures that reimbursement rates, billing terms, and payment schedules are accurately reflected in agreements, reducing claim denials and revenue leakage while improving cash flow.
What are the benefits of using contract lifecycle management software in healthcare?
Using CLM software streamlines contract drafting, approval, and monitoring processes. It also enhances compliance tracking, reduces administrative workload, and provides better visibility into contract performance and obligations.
What should you do next?
Thanks for reading till the end. Here are 3 ways we can help you automate your business:

Do better workflow automation with Cflow
Create workflows with multiple steps, parallel reviewals. auto approvals, public forms, etc. to save time and cost.

Talk to a workflow expert
Get a 30-min. free consultation with our Workflow expert to optimize your daily tasks.

Get smarter with our workflow resources
Explore our workflow automation blogs, ebooks, and other resources to master workflow automation.