Chronic Disease Management Program Approvals
Why automate?
How Cflow Can Help Automate the Process:
Automated Program Eligibility Verification:
Cflow automates the verification of chronic disease management program requests by cross-referencing the employee’s health condition and treatment needs against the policy terms. This ensures that only eligible programs are approved, reducing the risk of errors and speeding up the approval process, allowing employees to access essential disease management services promptly.
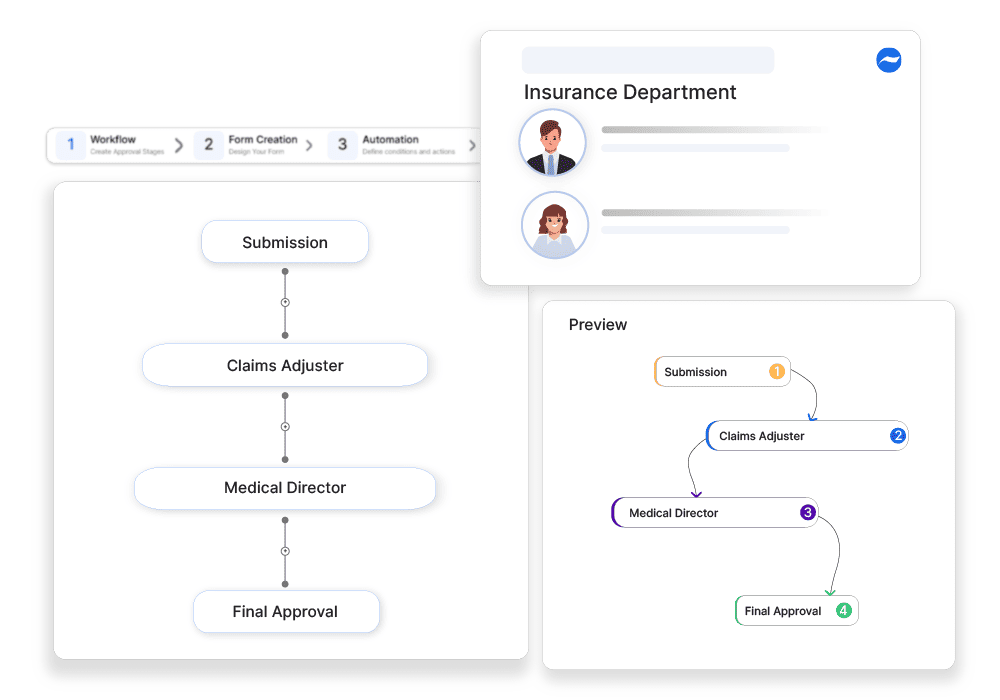
Customized Workflow Templates:
Cflow’s customizable workflow templates allow insurers and benefits administrators to create tailored workflows for chronic disease management program approvals. These workflows can include automated steps for document submission, eligibility verification, and final approval, ensuring that each request is processed efficiently and in accordance with policy guidelines.
Compliance and Regulatory Management:
Chronic disease management program approvals must comply with various legal and healthcare regulatory requirements, and Cflow helps insurers stay compliant by incorporating automated compliance checks into the approval process. This ensures that each request meets legal obligations, reducing the risk of non-compliance and potential legal issues.
Real-Time Tracking and Reporting:
With Cflow’s real-time tracking and reporting features, insurers and benefits administrators can monitor the progress of chronic disease management program requests at every stage. This visibility allows managers to quickly identify and resolve any issues, ensuring that requests are processed without unnecessary delays. Real-time reporting also enhances transparency, enabling insurers to keep employees informed about the status of their program approvals.
Frequently Asked Questions
What is a chronic disease management program?
A healthcare initiative that provides long-term care and monitoring for patients with chronic illnesses like diabetes or hypertension.
What are the main challenges in program approvals?
Strict eligibility requirements, documentation complexities, and inconsistent payer policies.
How can businesses improve chronic disease management program approvals?
By automating eligibility checks, ensuring accurate documentation, and implementing clear approval workflows.



