Patient Insurance Pre-authorization
Why automate?
How Cflow Can Help Automate the Process:
Streamlined Submission Process:
Cflow offers a simplified and user-friendly platform for submitting pre-authorization requests, ensuring that all required information is captured accurately and efficiently. This reduces the time and effort required to initiate a request.
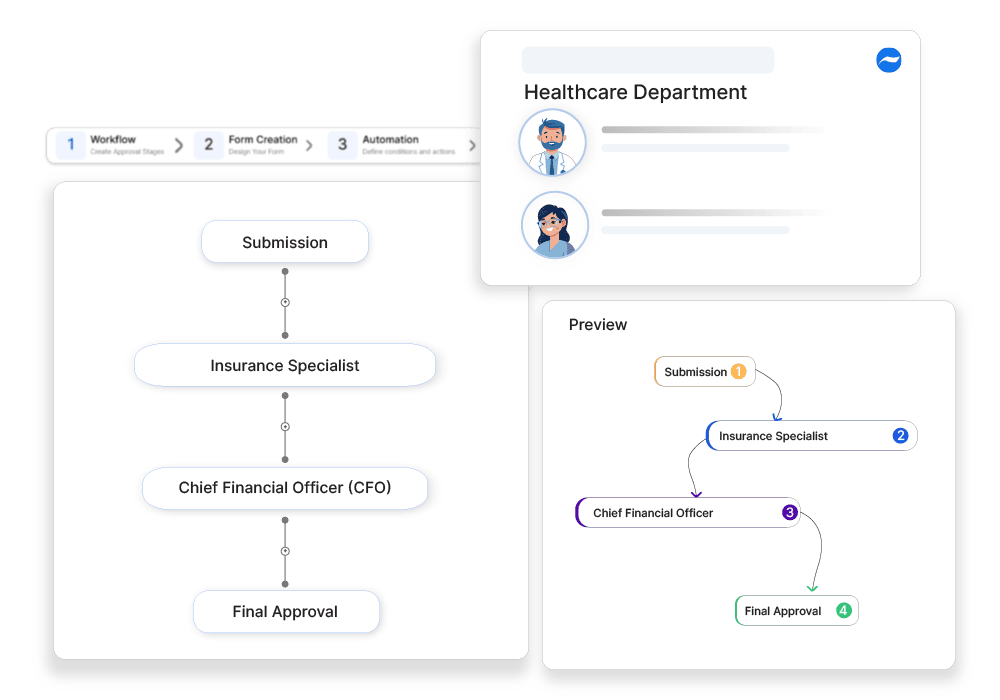
Automated Workflow Routing:
With Cflow, pre-authorization requests are automatically routed to the appropriate insurance representatives for review and approval. This eliminates manual handoffs and accelerates the approval process.
Real-time Status Updates:
Cflow provides real-time tracking of pre-authorization requests, allowing healthcare providers to monitor the status of each request at any time. This transparency ensures that all parties are informed and reduces the risk of delays.
Compliance and Documentation:
Cflow maintains detailed records of all pre-authorization requests, including submission details, approval actions, and communication logs. This comprehensive documentation supports regulatory compliance and provides valuable insights for future reference.
Frequently Asked Questions
Why is pre-authorization required for medical treatments?
To confirm coverage and avoid unexpected costs for patients.
What types of services typically require pre-authorization?
Surgeries, imaging scans, and specialized treatments.
How long does the pre-authorization process take?
It varies but typically takes 1-5 business days.



