Healthcare Provider Credentialing Approvals
Why automate?
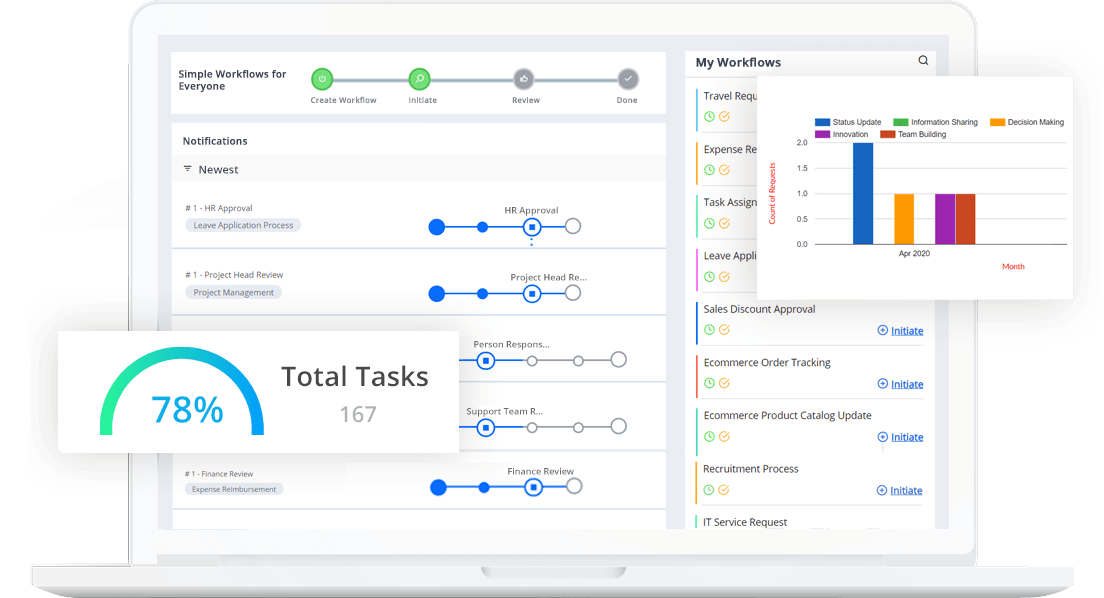
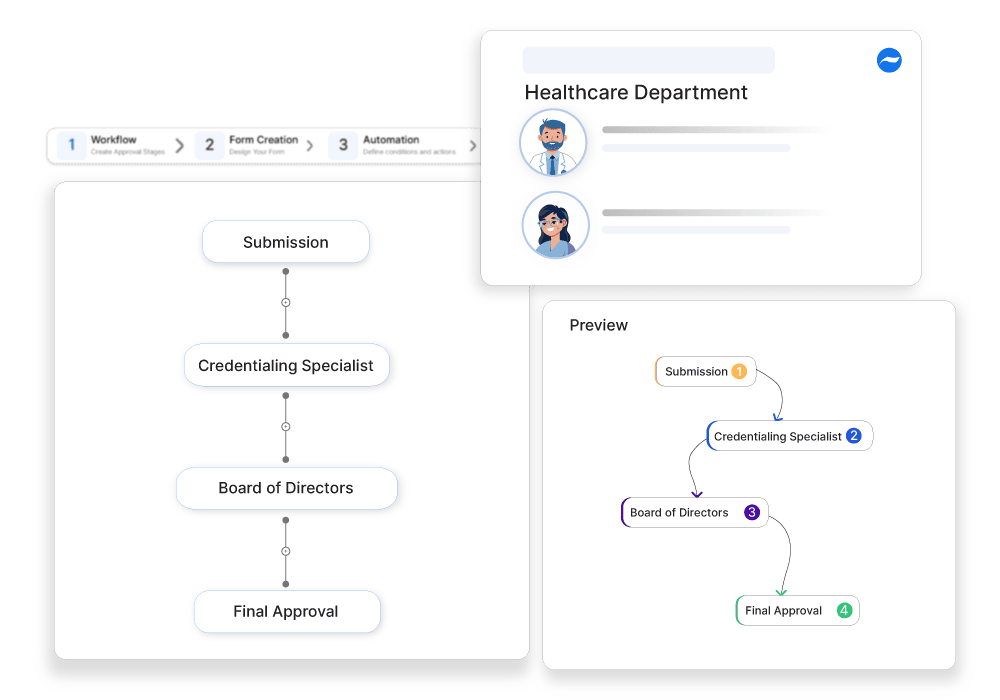
How Cflow Can Help (100 words each):
Automate Documentation Verification:
Cflow automates the verification of required documentation, ensuring that all provider credentials are up-to-date and compliant with regulatory standards.
Streamline Background Checks:
With Cflow, background checks and reference verifications can be automated, reducing the time and effort required to complete the credentialing process.
Enhance Compliance Tracking:
Cflow ensures that all credentialing activities are documented and compliant with healthcare regulations, reducing the risk of non-compliance and legal issues.
Reduce Processing Times:
By automating the credentialing workflow, Cflow significantly reduces the time taken to approve healthcare providers, enabling quicker onboarding and service delivery.
Frequently Asked Questions
What is healthcare provider credentialing?
A process that verifies a provider’s qualifications, experience, and compliance before allowing them to practice.
What are the main challenges in credentialing approvals?
Time-consuming verification, incomplete documentation, and regulatory changes.
How can businesses expedite healthcare provider credentialing approvals?
By using automated credential verification, real-time tracking, and compliance management tools.